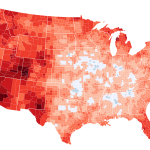
The critical shortage of organs available for transplant is a stark reality, leaving over 100,000 Americans on waiting lists, with 13 dying each day. While a significant majority—around 60% of eligible adults—have registered as organ donors, the gap between intention and action highlights a complex issue demanding closer examination. This disparity isn’t simply about apathy; it’s a consequence of systemic challenges and individual considerations that undermine even the most well-meaning intentions.
The Two Sides of Donation: After-Death and Living Donation
The system of organ donation hinges on two distinct approaches: donation after death and living donation. Donation after death, often signified by an organ donor designation on a driver’s license, relies on the timely retrieval of organs following a person’s demise. However, this process is fraught with complexities. Firstly, the timing must be precise. Organs must be harvested within a narrow window after death to remain viable for transplantation. This necessitates a rapid and efficient system of notification, coordination between hospitals and organ procurement organizations (OPOs), and a seamless process of organ retrieval. Any delay, even a small one, can render the organs unusable, leading to a tragic loss of potential life-saving opportunities. Furthermore, the cause of death plays a crucial role. Not all deaths result in organs suitable for transplantation. Traumatic injuries, certain infections, and extensive damage can render organs unsuitable, regardless of the donor’s registered status.
Living donation, on the other hand, involves a person voluntarily donating a kidney or part of their liver while still alive. While a more immediate solution, this process is governed by strict ethical and medical guidelines, ensuring donor safety and well-being. The decision to donate a vital organ is deeply personal and carries significant risks, requiring extensive medical evaluations and counseling to assess both physical and psychological suitability. The altruism of living donors is indispensable, but the limited pool of potential donors and the inherent medical risks associated with the procedure significantly constrain the number of transplants possible through this method.
Addressing the Systemic Bottlenecks
Beyond the individual complexities of donation, systemic issues also hinder the process. These issues include:
*
Lack of public awareness:
While many support organ donation, the intricacies of the process and the crucial role of timely consent are often misunderstood. Increased public education campaigns could significantly improve registration rates and ensure that families are well-informed about their loved one’s wishes.
*
Inefficient systems:
The system for organ procurement and allocation can be cumbersome and inefficient, leading to delays and missed opportunities. Improvements in technology and coordination among healthcare institutions are crucial to streamlining the process.
*
Ethical and logistical challenges:
The allocation of scarce organs raises complex ethical questions about fairness and prioritization. Ensuring equitable access to transplantation remains a major challenge.
Conclusion: A Call for Collaborative Action
The organ shortage isn’t merely a medical problem; it’s a societal one, demanding a multi-faceted approach. By improving public awareness, streamlining the donation process, addressing systemic inefficiencies, and fostering open conversations about end-of-life choices, we can bridge the gap between good intentions and life-saving action. The solution lies in collaborative efforts involving healthcare professionals, policymakers, and the public, working towards a future where organ donation becomes a more effective and accessible system that saves countless lives.
Based on materials: Vox